Hemophilia Landscape Emerging Therapies
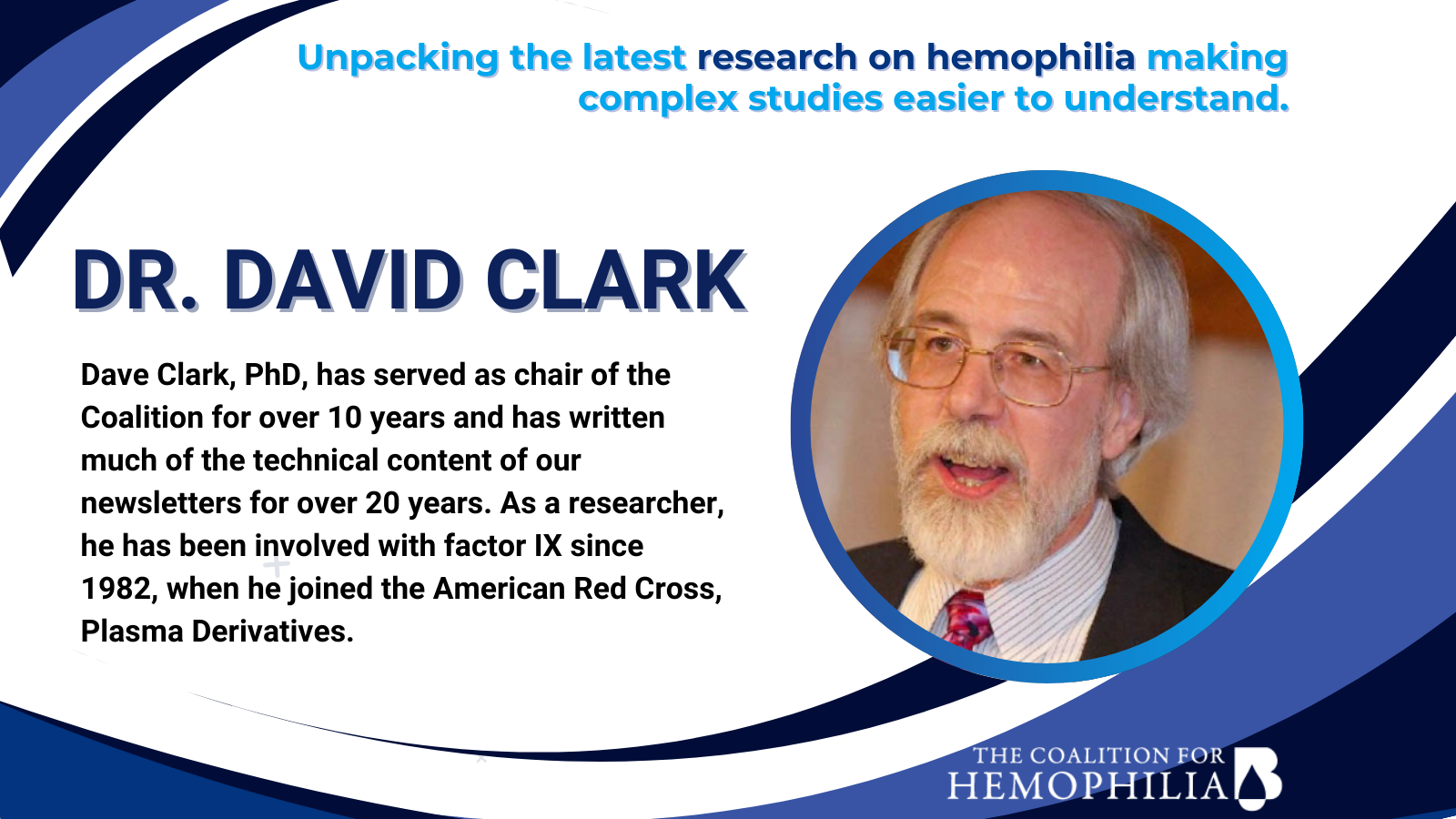
By Dr. David Clark
Hemophilia Landscape Emerging Therapies
By Dr. David Clark
There is a huge amount of new product development going on in hemophilia B. The potential new products can be separated into three categories, 1) improved factor products, 2) rebalancing agents and 3) gene therapy. These updates are divided into those three categories. Within each category, the entries are generally listed in order of the names of the organizations developing the product.
A number of the items below were presented at the annual congress of the European Association for Haemophilia and Allied Disorders (EAHAD), February 6 – 9, 2024 in Frankfurt, Germany.
IMPROVED FACTOR PRODUCTS
These are improved versions of the factor products that most people with hemophilia B are currently using, also including products for inhibitor treatment. The improvements include longer half-lives and delivery by subcutaneous injection. This section also includes updates on some of the current products on the market.
FDA Approves Pediatric Indication for Ixinity
3/22/24 Medexus Pharma’s Ixinity received approval from FDA to expand their indication to include children younger than 12 years of age. The indication includes on-demand treatment, prophylaxis and use during surgery. Ixinity is now approved for all patients with hemophilia B. The approval was based on a Phase III/IV study of use in children. [FDA approval letter to Medexus 3/22/24]
Ixinity is slightly different from the other standard half-life factor IX products on the U.S. market. Benefix and Rixubis both have a factor IX protein that includes the amino acid alanine at the 148th position in the protein chain, designated ala148. (A protein is a long chain of amino acids strung together.) Ixinity has the amino acid threonine (three – o – neen) in the 148th position, designated thr148. These are called isoforms, and both appear in plasma. Different populations have different relative amounts of the two isoforms. Because they are purified from large pools of plasma, plasma-derived products like Alphanine contain both isoforms, and often others.
In the laboratory, there is no significant difference between the two isoforms in terms of bioactivity, but in patients in real life, there does appear to be some difference in some people. Some people seem to respond better to Ixinity and others are better with Benefix/Rixubis. For most people, though, all three products work fine. Therefore, if you are not getting good results with your factor IX product, you might want to talk to your doctor about trying a product with the other isoform. [Graham JB et al., Am J Hum Genet, 42:573-580, 1988]
Do Recombinant Products Cause Higher Levels of Inhibitor Development?
2/8/24 The SIPPET study published in 2016 caused a huge stir in the hemophilia community because it suggested that patients on plasma-derived factor VIII (for hemophilia A) products developed only about half the inhibitors as patients on recombinant products. However, there has been little follow-up to that study, which also did not include hemophilia B. An international group of researchers presented a new study at the European Association for Haemophilia and Allied Diseases (EAHAD) annual meeting.
In 1219 hemophilia A PUPs (previously untreated patients), they found an overall incidence of inhibitor development of 26%. The study confirmed the SIPPET results but found smaller differences between plasma-derived and recombinant products. The patients on plasma-derived products had a 20% chance of developing an inhibitor, while those on standard half-life (SHL) recombinants had a 27% chance. Extended half-life (EHL) products came between those at 22%.
In 173 PUPs with hemophilia B, there were no significant differences among the products. Plasma-derived products had an 11% risk of inhibitor development; SHL products came in at an 8% risk and EHL products were at 7%. Although the averages for B appear different, there was a large amount of overlap in the results, so no significant differences were observed. [EAHAD abstract PO129]
REBALANCING AGENTS
Rebalancing agents tweak the clotting system to restore the balance so the blood clots when it should and doesn’t clot when it shouldn’t. The clotting system is a complex system of clotting factors that promote clotting and anticoagulants that inhibit clotting. In a person without a bleeding disorder, the system is in balance, so it produces clots as needed. In hemophilia, with the loss of some clotting factor activity, the system is unbalanced; there is too much anticoagulant activity keeping the blood from clotting. Rebalancing agents mainly reduce or inhibit the activity of anticoagulants in the system. Most of these agents work to help restore clotting in people with hemophilia A or B, with or without inhibitors.
Centessa Presents Updates on SerpinPC
2/9 and 5/13/24 Centessa is developing SerpinPC, an inhibitor of the anticoagulant activated protein C (APC) as a rebalancing agent. SerpinPC is a biweekly or monthly subcutaneous injection for treatment of hemophilia A and B patients, with or without inhibitors. Centessa presented updates on their Phase IIa clinical studies at the American Society of Hematology (ASH) meeting in December and at EAHAD.
Over 2.8 years, they found a significant decrease in annualized bleeding rate (ABR), which declined from a median of 35.6 before treatment to 1.0 after SerpinPC. Note that the pre-treatment ABR was high because the subjects were all treated on-demand rather than with prophylaxis before the study (at baseline). All 20 subjects (16 As, 4 Bs) had target joints at baseline, but only two still had target joints at the end of the study. The product was well-tolerated with no treatment-related adverse effects. They found no evidence of thrombosis (too much clotting). This is the ongoing Part 1 of Centessa’s studies. By the end of 2024, they plan to have confirmed the optimum dose and be ready to move to the next phase of the trials. [Centessa press releases, 2/9/24 and 5/13/24]
Novo Nordisk Presents Updates on Concizumab
2/9/24 Novo Nordisk is developing concizumab, an inhibitor of the anticoagulant tissue factor pathway inhibitor (TFPI) as a rebalancing agent. Concizumab is a daily subcutaneous injection for treatment of hemophilia A and B patients, with or without inhibitors. Novo presented updates on their Phase III clinical studies at EAHAD.
Novo gave an update of the Phase III study results after all patients had been treated for 56 weeks. The subjects included 80 As (HA) and 64 Bs (HB) without inhibitors plus 76 As (HAwI) and 51 Bs (HBwI) with inhibitors. They found median annualized bleeding rates (ABRs) of 0.7 (range 0.0 to 3.0) for HAwI, 1.1 (0.0 - 3.2) for HBwI, 1.7 (0.0 – 4.5) for HA and 2.8 (0.0 – 6.4) for HB. Although it seems that there is a variation among the different groups, the ranges overlap, so the differences may not be significant. FDA had previously put a clinical hold on the studies because of thrombosis in a few patients. After that, Novo revised the protocol and dosing to FDA’s satisfaction, and restarted the studies. There were no additional thromboembolic complications from the restart to the 56-week analysis. [EAHAD abstract OR07]
Novo also presented results for concizumab patients who had surgery during the clinical studies. Major surgeries were prohibited in the studies, but minor procedures were allowed. Thirty patients (out of 278 total) had minor surgeries. This included nine As and ten Bs without inhibitors, plus seven A and four B inhibitor patients. Surgery-related excess bleeding occurred in 14 out of 38 total procedures, and eight were treated with factor. Only one bleeding episode was severe. The median duration of bleeding was two days and the average number of factor injections per patient was 1.5. The surgeries included 24 dental procedures. The others included port removal, colonoscopy, joint fusion and urethral augmentation. [EAHAD abstract PO064]
One of the issues with the rebalancing agents is testing patients to determine whether they have effective levels of the product. Since these products don’t contain factor VIII or IX, a test for factor levels is not feasible. What is needed is a test for the overall coagulability of the blood. This has been an ongoing problem in hemophilia as scientists have developed advanced treatments for which measurements of factors VIII or IX are not sufficient. One possibility is the rotational thromboelastometry or ROTEM test, which measures the strength and elasticity of a clot as it forms in a blood sample. However, the Novo group found that ROTEM is not suitable for monitoring of clotting potential with concizumab.
Novo is to be congratulated for publishing this. Although scientists are encouraged to publish all of their work, not just the successful parts, it rarely happens that they publish negative results – experiments that don’t work. Negative results are still knowledge. Knowing what doesn’t work can help us better understand what might work. It also keeps research groups from wasting time exploring the same rabbit hole over and over. [EAHAD abstract PO021]
Pfizer Updates on Marstacimab
2/8/24 Pfizer is developing marstacimab, an inhibitor of the anticoagulant tissue factor pathway inhibitor (TFPI) as a rebalancing agent. Marstacimab is a once-weekly subcutaneous injection delivered via an auto-injector pen for treatment of hemophilia A and B patients, with or without inhibitors. They presented two papers at EAHAD.
The first paper looked at data from their Phase III study concerning joint health. In 123 patients without inhibitors, they saw significant reductions in joint bleeds, joint status (decreases in the Hemophilia Joint Health Score (HJHS), where a lower result is better) and the number of target joints. (The results are difficult to summarize because they are presented independently from several different studies, but all of the groups saw similar improvements.) [EAHAD abstract PO074]
In the second paper, they looked at the development of anti-drug antibodies (ADAs) against marstacimab, again in patients without inhibitors. ADAs against factor IX or factor VIII are called inhibitors in hemophilia. Other drugs can also have similar antibody reactions to the drug. ADAs are generally divided into two categories, neutralizing and non-neutralizing. Neutralizing antibodies interfere with the performance of the drug, while non-neutralizing ADAs may bind to the drug, but don’t interfere with its function. They found that most ADAs were low and transient, that is, they disappear after a while, in this study within about two months. No patients were ADA-positive by the end of the study. ADAs did not appear to interfere with the treatment or change the incidence of adverse events. [EAHAD abstract PO186]
TiumBio Submits Application for Phase Ib Studies of TU7710 for Inhibitor Patients
3/26/24 TiumBio, a Korean biotech, is developing TU7710, a longer-acting activated factor VII (FVIIa) product for treatment of hemophilia A and B patients with inhibitors. TU7710 consists of FVIIa molecules fused to the protein transferrin. This gives TU7710 a half-life about six to seven times longer than NovoSeven. TiumBio is currently conducting a Phase Ia study evaluating the safety, tolerability and pharmacokinetics (PK) of TU7710 in healthy male volunteers (without inhibitors), with results expected by mid-2024.
TiumBio has now submitted a Clinical Trial Application (CTA) for a Phase Ib study. (A CTA is the European version of the US FDA’s IND for approval to conduct a study in humans.) The Phase Ib study will continue the safety/tolerability/PK studies in inhibitor patients. It will also look at various dosage levels to determine the dosage for a subsequent Phase II study. [TiumBio press release 3/26/24]
Gene and Cell Therapy
Gene therapy is the process of inserting new, functional factor IX genes into the body to allow it to produce its own factor IX. Cell therapy is the transplantation of whole cells that have been modified to perform a specific function such as producing factor IX.
Gene Therapy for Inhibitor Patients?
2/9/24 Hemophilia patients with inhibitors are not eligible for the current gene therapy treatments for hemophilia A or B. Hemophilia B inhibitor patients produce antibodies against factor IX when it is given by infusion. So, what would happen if a B inhibitor patient were given one of the two approved gene therapies? Two scenarios are possible. In the worst case, their body would start producing new factor IX molecules, but the immune system would still try to eliminate the new factor IX from the body. This would set up a “war” between the immune system and the liver, where the new factor IX is produced. This could be a dangerous, even life-threatening, condition. The best case is that the gene therapy would act like immune tolerance induction (ITI) in which an inhibitor patient is given frequent high doses of factor to induce the body to learn to tolerate it. We don’t know which will happen.
Biomarin, who produces Roctavian, a gene therapy for hemophilia A, decided to find out. In a Phase I/II study approved by FDA, they gave Roctavian to four hemophilia A inhibitor patients. The first two patients had current inhibitor levels of 3.8 and 2.2 BU/ml, respectively. Patient 1’s inhibitor levels increased for twelve weeks, but started down after that point. However, he then developed an inflamed liver that was treated with corticosteroids, the normal treatment for liver inflammation after gene therapy. His inhibitor level rose after that. Patient 2 had an inhibitor level that rose to 20.1 BU/ml at nine weeks, but then declined to <0.6 BU/ml, indicating that the inhibitor had been eliminated. At that point, his factor VIII level had risen to 41.7%.
Two other patients, who had had inhibitors that were previously eliminated by ITI, had levels of <0.6 BU/ml before gene therapy treatment. Their factor VIII levels rose to 26.2 and 249% after gene therapy. (Note that 249% is too high and might induce thrombosis, dangerous unneeded clotting.) Neither of their inhibitor levels rose after treatment. No serious or severe adverse events were reported in any of the four patients. The patients did not appear to have any different safety responses than the non-inhibitor patients in the Roctavian clinical studies.
This was an early report from an ongoing study in hemophilia A that was presented at EAHAD, but it provides a glimmer of hope for hemophilia B inhibitor patients. Researchers have also seen elimination of inhibitors by gene therapy in animals, but this is the first human experience. Much more research will be required, but one day, hemophilia inhibitors may be a thing of the past. [EAHAD abstract OR10]
CSL Reports on Hemgenix Gene Therapy after Three and Four Years
2/9/24 CSL Behring markets Hemgenix, a gene therapy for hemophilia B that is delivered by an adeno-associated virus (AAV) vector and uses the Padua high-activity factor IX gene. At EAHAD, they presented updates on patient results after three years in their Phase III study and after four years in their Phase IIb study. From the Phase III study, 52 of the original 54 subjects completed a three-year follow-up. Their mean (average) ABR for all bleeds was 1.52, compared with 4.17 during the 6-month pre-treatment period when they were on conventional prophylaxis. Their mean factor IX levels were 41.5% of normal one year after treatment, 36.7% after year two and 38.6% after year three. (Note that the standard deviations for these values are fairly large, so there is no evidence that the levels are decreasing.) Fifty-one subjects have discontinued prophylaxis, but one subject had his factor IX levels decline to the 2 – 5% range, resumed prophylaxis and his bleeds returned. [EAHAD abstract OR09]
From their earlier Phase IIb study, which included only three subjects, mean factor IX levels were 31% at 6 weeks after treatment, 40.7% at one year, 44.2% after two years, 36.9% at year three and 45% at year four. The ABR was 0.22 at year three and 0.17 at year four. [EAHAD abstract PO038]
CSL Reports on Quality of Life after Two Years on Hemgenix
3/10/24 CSL published a report on the quality of life (QoL) for patients in their Phase III clinical study of Hemgenix after two years. The study used various questionnaires and compared results from six months before treatment and two years after treatment. On the Hem-A-Qol questionnaire, the categories (domains) of Treatment, Feelings, Work/School and Future showed improvement, while the other categories did not. [Itzler R et al., Haemophilia, online ahead of print 3/10/24]
Frontera Reports Pre-Clinical Results for FT-004
5/9/24 Frontera Therapeutics is developing FT-004, a gene therapy for hemophilia B that is delivered by an adeno-associated virus (AAV) vector and uses the Padua high-activity factor IX. At the American Society of Cell and Gene Therapy (ASGCT) annual meeting, they presented pre-clinical animal data for FT-004. Their key improvement is to eliminate CpG sequences in the new factor IX gene in order to minimize the immune response to their treatment. CpG sequences are a cytosine base followed by a guanine base in the DNA sequence of a gene. Previous research has suggested that CpG sequences activate the immune system, and thus may affect the efficiency of insertion of the new gene.
FT-004 was tested in both hemophilia B mice and in cynomolgus monkeys, giving good results in both. They saw high factor IX expression and no apparent safety issues in the animals. [ASGCT abstract 1088]
Pfizer’s Beqvez Gene Therapy Approved by FDA
4/25/24 Pfizer has been developing Beqvez (fidanacogene elaparvovec), a gene therapy for hemophilia B that is delivered by an adeno-associated virus (AAV) vector and uses the Padua high-activity factor IX gene. They have now received FDA approval to market Beqvez in the U.S. with the following indication:
BEQVEZ is an adeno-associated virus vector-based gene therapy indicated for the treatment of adults with moderate to severe hemophilia B (congenital factor IX deficiency) who:
Currently use factor IX prophylaxis therapy, or
Have current or historical life-threatening hemorrhage, or
Have repeated, serious spontaneous bleeding episodes, and,
Do not have neutralizing antibodies to adeno-associated virus serotype Rh74var (AAVRh74var) capsid as detected by an FDA-approved test.
This is essentially the same as the indication for Hemgenix, CSL’s competing factor IX gene therapy, with the exception that Hemgenix doesn’t have a limitation on pre-existing antibodies to their vector AAV5. At the same time, FDA approved a test for antibodies against the AAVRh74var vector. Neither product may be used for patients with inhibitors or a history of inhibitors, and neither is intended for use in women.
Beqvez was developed by Pfizer and Spark Therapeutics, which is now a subsidiary of Roche. Pfizer has set a list price of $3.5 million, matching Hemgenix. (Hemgenix was once the most expensive pharmaceutical in the world, but this was recently surpassed by Orchard Therapeutics’ Lenmeldy gene therapy for metachromatic leukodystrophy, which has a price of $4.25 million.) [FDA approval letter 4/25/24 and Pfizer communications]
Pfizer Presents Updates on Beqvez
2/9/24 Pfizer presented three papers at EAHAD on Beqvez. The first paper looked at health-related quality of life (HRQoL) in subjects who received Beqvez in the clinical studies. The 42 subjects with a median age of 29 (range 18 – 62) at the time of treatment, completed a number of questionnaires both before treatment and at the one-year mark. On the often-used Haemophilia Quality of Life Questionnaire for Adults (Haem-A-QoL) the average drop one year after treatment was 11.2 points, a significant improvement in HRQoL where lower scores are better. They also saw improvements in other aspects including physical health, feelings, view of self, work/school, sport/leisure, treatment and future outlook. [EAHAD abstract PO116]
Pfizer also reported on clearance of the gene therapy vector from the body in the patients in their Phase III study. They looked at vector DNA levels in plasma, peripheral blood mononuclear cells (PBMC, a type of white blood cell), semen, saliva and urine. Complete clearance of the DNA was achieved within an average of 1 – 4 months, except in PBMCs, which took up to seven months. [EAHAD abstract PO132]
Finally, they looked at what doses of an extended half-life (EHL) product like Alprolix would be needed to match the factor IX trough levels provided by Beqvez over the course of 25 years. They assumed that the factor level provided by Beqvez would decline somewhat over the 25 years, a conservative estimate since we don’t know how long gene therapy will continue to provide adequate factor levels. For a fixed weekly dosing regimen, the study estimates that Alprolix doses of 251, 174, 117, and 47.8 IU/kg would be required in years 1, 5, 10 and 25. If, instead, the Alprolix dose were fixed at 50 IU/kg, the estimated dosing frequencies would be every 2.72, 3.42, 4.35, and 7.18 days in years 1, 5, 10 and 25. These results demonstrate how high a dose or how often an infusion would be required to match the factor levels provided by Beqvez. This helps to support the cost-effectiveness of gene therapy over traditional factor infusions. [EAHAD abstract PO182]
Regeneron to Continue Work on Gene Therapy for Hemophilia B
3/22/24 Regeneron Pharmaceuticals and Intellia Therapeutics have been developing a gene editing treatment for hemophilia B. The companies received approval for their Phase I clinical study, which is scheduled to begin in mid-2024. However, Intellia has decided to end its collaboration with Regeneron on the project. Regeneron will continue the project on its own. The treatment uses CRISPR/Cas9 technology to insert a new factor IX gene into the genome of liver cells. [Hemophilia News Today article 3/27/24]